Many people are curious about what happens behind the scenes when they visit a doctor with a new health concern. Why does your doctor order some tests but not others? How do they decide which tests to start with, and why aren’t all possible tests done at once? Understanding this process can help you feel more confident and informed during your medical journey. In this article, we explore how doctors make these important decisions, focusing on symptoms, cost considerations, the stepwise approach to diagnostics, and the reasons behind not testing for everything immediately.
How symptoms guide testing
Your symptoms are usually the first and most important clue in the medical evaluation. When you describe what you are experiencing—such as pain, fever, fatigue, or a specific change in your body—your doctor listens carefully and asks targeted questions to better understand your situation. This process is called taking a medical history.
Doctors use your symptoms, along with your medical history and a physical examination, to form what is called a “differential diagnosis.” This is a list of possible conditions that could explain your symptoms. The aim is to narrow down this list as efficiently as possible, starting with the most likely or most serious possibilities.
- For example, if you have chest pain, a doctor will consider heart, lung, digestive, and musculoskeletal causes.
- If you come in with a sore throat, the doctor will look for signs of viral or bacterial infections, allergies, or other causes.
The initial tests ordered are usually those that can quickly confirm or rule out the most urgent or probable conditions. This approach helps ensure your care is both safe and effective, while avoiding unnecessary tests that may not be helpful.
Cost vs necessity
Healthcare resources—both financial and technical—are not unlimited. Doctors must balance the need to make an accurate diagnosis with the responsibility to avoid wasteful or excessive spending. Each test has a cost, not only in terms of money, but also in time, potential discomfort, and the possibility of false alarms that may lead to further unnecessary testing.
- Some tests are expensive and may only be used if they are very likely to provide important information.
- Insurance coverage or national health system guidelines may influence which tests are available or recommended first.
- Doctors are trained to consider which test is the most efficient and cost-effective for each situation.
Doctors must also consider the value of the information a test will provide. A test is only necessary if its results are likely to change the course of your care—such as confirming a diagnosis, ruling out a dangerous condition, or helping to choose the best treatment. If a test is unlikely to provide useful information, it is generally not ordered, even if it is available.
Risks associated with unnecessary testing
Every test, even simple blood tests, carries some risk. For example, imaging tests may expose you to radiation, and invasive procedures can lead to infection or other complications. Over-testing can also lead to “false positives”—results that suggest a problem when there isn’t one, potentially leading to anxiety or unnecessary further procedures. Cost is not just a matter of money; it is also about your safety and well-being.
Stepwise diagnostics
Doctors often use a step-by-step approach to diagnosis, known as “stepwise diagnostics.” This means that they start with basic tests that are likely to provide the most information with the least risk or cost. Based on those results, further testing may be considered if needed.
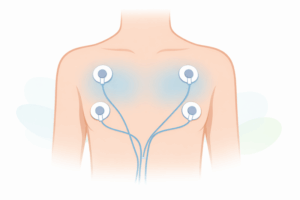
- Initial tests might include basic blood tests, urine analysis, or a chest X-ray.
- If these tests are inconclusive or suggest a more serious problem, more advanced or specialised tests may follow.
- Sometimes, the diagnosis can be made after the first round of testing, and no further tests are necessary.
This approach helps avoid unnecessary testing and ensures that each step is guided by new information. Doctors may also use “watchful waiting” in some cases, monitoring your symptoms over time to see if the picture becomes clearer without immediate testing.
Examples of stepwise testing in practice
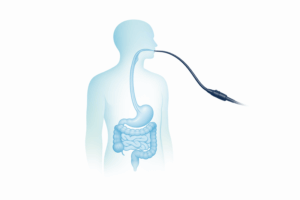
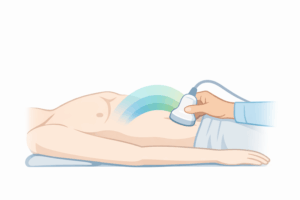
- Abdominal pain: A doctor may begin with a physical exam and simple blood tests. If these suggest a specific condition, such as appendicitis, imaging like an ultrasound or CT scan might be ordered next.
- Headaches: Most headaches are not caused by serious conditions. Doctors may start with a medical history and neurological exam. Imaging tests like MRI or CT are reserved for cases with warning signs or unusual features.
Why not everything is tested at once
It is a common misconception that doctors should “test for everything” just to be safe. In reality, this approach is neither practical nor safe. There are several important reasons why not all possible tests are ordered immediately:
- Volume of possible tests: The number of available medical tests is enormous. Testing for everything would be overwhelming and unmanageable, both for patients and for the healthcare system.
- Risk of misleading results: The more tests you have, the higher the chance of encountering false positives, leading to confusion and unnecessary worry.
- Physical burdens: Some tests require fasting, injections, or other preparations that can be uncomfortable or disruptive.
- Resource allocation: Healthcare systems must use resources wisely to ensure that everyone can access the tests they truly need.
Instead, doctors focus on the most likely or most dangerous conditions first. This approach is guided by medical guidelines, experience, and ongoing research into the most effective ways to diagnose and treat patients.
Personalising the approach for each patient
No two patients are exactly the same. Factors like age, medical history, family history, and current medications can influence which tests are appropriate. Doctors take all these into account, aiming to tailor the diagnostic process to your individual needs and circumstances.
Open communication with your doctor is key. If you are worried about a specific condition or test, or if you feel something important has not been considered, share your concerns. Your doctor can explain their reasoning and, if appropriate, discuss the possibility of further testing.
Conclusion: A partnership in care
The process of deciding which tests to order is both a science and an art. Doctors rely on their training, experience, and the latest medical evidence to guide their decisions, always keeping your safety and well-being in mind. By understanding how this process works, you can be an informed and active participant in your own care.
If you are interested in learning what doctors typically look for when reviewing initial blood test results, you can read more in our detailed guide on what doctors check first in blood test results.
If you ever have questions about your tests or the reasoning behind your doctor’s choices, do not hesitate to ask. Working together with your healthcare team ensures the best possible outcomes and peace of mind throughout your diagnostic journey.