Type 2 diabetes is a common condition that affects how your body processes blood sugar (glucose). It often develops gradually, with subtle symptoms that can be easy to overlook. Recognising the early signs and understanding what to expect from the diagnostic process can help you take control of your health sooner. This article explains the early warning signs, risk factors, how diabetes is diagnosed, and what usually happens after a diagnosis.
Subtle early signs
The early stages of type 2 diabetes may not cause obvious symptoms. Many people are unaware they have the condition until it is picked up during routine blood tests. However, some early warning signs can include:
- Increased thirst and frequent urination: High blood sugar causes your kidneys to work harder to filter and absorb the excess glucose, which can lead to more trips to the toilet and feeling thirsty more often.
- Fatigue: If your body cannot use glucose efficiently for energy, you may feel unusually tired or lacking in energy throughout the day.
- Blurred vision: High glucose levels can cause swelling in the lens of your eye, leading to temporary changes in your vision.
- Slow-healing wounds or frequent infections: High blood sugar can affect your body’s ability to heal and fight off infection, so cuts may take longer to heal and you might notice more frequent infections, especially of the skin, gums, or urinary tract.
- Unintended weight loss: Although more common in type 1 diabetes, some people with type 2 diabetes may lose weight without trying as the body starts to break down muscle and fat for energy.
- Tingling or numbness in hands or feet: Over time, high blood sugar can damage nerves, leading to sensations such as tingling, numbness, or pain, especially in the extremities.
- Darkened skin patches: Some people develop dark, velvety areas of skin, usually in the folds and creases of the body, such as the neck and armpits. This is known as acanthosis nigricans and can be a warning sign of insulin resistance.
Because these symptoms can be mild and develop slowly, they are often mistaken for normal aging or daily stress. If you notice any of these changes, especially if you have risk factors for diabetes, it’s important to speak to your healthcare provider.
Risk factors
Anyone can develop type 2 diabetes, but certain factors increase your risk. Understanding these risk factors can help you and your doctor decide whether you should be screened for the condition.
- Family history: Having a parent or sibling with type 2 diabetes increases your risk.
- Age: The risk rises as you get older, especially after age 45, although it is increasingly being diagnosed in younger people.
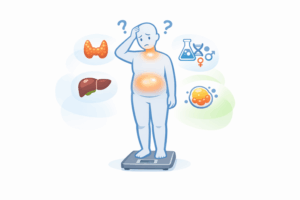
- Weight: Being overweight or having obesity is one of the strongest risk factors, particularly if you carry excess weight around your abdomen.
- Physical inactivity: Regular physical activity helps your body use insulin more efficiently. A sedentary lifestyle increases your risk.
- Ethnicity: People of South Asian, African-Caribbean, Middle Eastern, or East Asian descent are at higher risk, even at lower body weights.
- High blood pressure and cholesterol: Having high blood pressure or abnormal cholesterol levels can also increase risk.
- History of gestational diabetes: Women who developed diabetes during pregnancy have a higher risk of developing type 2 diabetes later in life.
- Polycystic ovary syndrome (PCOS): Women with PCOS are at increased risk, possibly due to insulin resistance.
Other factors, such as sleep disorders, smoking, and certain medications, can also play a role. If you have one or more of these risk factors, ask your doctor about your risk and whether testing is appropriate for you.
How diabetes is diagnosed
If your doctor suspects you may have type 2 diabetes, either because of symptoms or risk factors, they will usually recommend blood tests to check your glucose levels. The most common tests used for diagnosis include:
- Fasting plasma glucose (FPG) test: This test measures your blood sugar after you have not eaten for at least eight hours (usually overnight). A fasting blood sugar level of 7.0 mmol/L (126 mg/dL) or higher on two separate occasions usually confirms diabetes.
- HbA1c test: Also known as the glycated haemoglobin test, this measures your average blood sugar level over the past two to three months. An HbA1c result of 6.5% (48 mmol/mol) or higher is considered diabetes.
- Oral glucose tolerance test (OGTT): This test involves fasting overnight, then drinking a sugary solution at the doctor’s office. Your blood sugar is measured before and two hours after the drink. A level of 11.1 mmol/L (200 mg/dL) or above after two hours is diagnostic for diabetes.
- Random plasma glucose test: If you have symptoms of diabetes, a blood sample may be taken at a random time, regardless of when you last ate. A level of 11.1 mmol/L (200 mg/dL) or higher suggests diabetes, especially if you are experiencing symptoms.
Sometimes, these tests may need to be repeated to confirm the result. Your doctor may also check for other health conditions that can be linked to diabetes, such as high cholesterol or high blood pressure.
Screening for diabetes is often recommended for people with risk factors, even if they do not have symptoms. Early detection allows for earlier management and can help prevent complications.
Pre-diabetes: an important warning
Some people have blood sugar levels that are higher than normal but not yet high enough to be diagnosed as diabetes. This is known as pre-diabetes (impaired glucose tolerance or impaired fasting glucose). If you are told you have pre-diabetes, it is a signal that you are at high risk of developing type 2 diabetes in the future. At this stage, lifestyle changes can have a significant impact and may even prevent diabetes from developing.
What usually happens after diagnosis
Being diagnosed with type 2 diabetes can be overwhelming, but you do not have to face it alone. After a diagnosis, your healthcare team will work with you to develop a personalised management plan. The main goals are to keep your blood sugar levels within a healthy range and prevent complications.
- Education and support: You will likely be offered education about diabetes, either one-to-one or in a group setting. This may cover healthy eating, physical activity, blood sugar monitoring, and how to look after your feet and eyes.
- Lifestyle changes: Making healthy changes to your diet and activity level can have a big impact. Your doctor or a dietitian may help you create a plan that fits your lifestyle and preferences.
- Medication: Some people can manage type 2 diabetes with lifestyle changes alone, especially if it is caught early. Others may need medication to help control blood sugar. Your doctor will explain your options and monitor your response over time.
- Regular check-ups: Ongoing monitoring is important. You will need regular blood tests to check your blood sugar, cholesterol, and kidney function. Your doctor will also check your blood pressure, weight, and foot health.
- Eye and foot care: Diabetes can affect your eyes and feet, so regular eye exams and foot checks are recommended.
- Support for emotional wellbeing: Living with a chronic condition can affect your mental health. Support is available from healthcare professionals, patient groups, and diabetes associations.
Managing diabetes is a lifelong process, but many people find that with support and education, they are able to live full and active lives. Over time, your management plan may need to be adjusted to suit your needs. If you have questions or concerns, do not hesitate to talk to your healthcare team.
If you are interested in learning more about how blood tests are used to check for diabetes and other conditions, you may find our detailed overview of what doctors look for in blood test results helpful.
Preventing complications
One of the most important reasons for early diagnosis and careful management is to prevent or delay complications. Uncontrolled diabetes can lead to problems with your heart, kidneys, eyes, nerves, and feet. However, by keeping your blood sugar, blood pressure, and cholesterol in check, you can reduce your risk.
Staying proactive
Type 2 diabetes does not have to control your life. By recognising the early signs, understanding your risk, and working closely with your healthcare team, you can take positive steps to manage your condition. If you are concerned about your risk or are experiencing any symptoms, book an appointment with your doctor. Early action can make a real difference.
Remember: The information in this article is for general guidance. Always consult your healthcare professional for advice tailored to your personal health situation.