A stroke is a medical emergency that can happen suddenly and without warning. Recognizing the signs early and acting quickly can save lives and prevent long-term disability. This article explains what a stroke is, how to spot the most common warning signs using the FAST method, other important symptoms to watch out for, what to do if you suspect a stroke, and what typically happens when a person is treated in the hospital.
Understanding stroke symptoms can help you react fast—whether it’s for yourself, a loved one, or even a stranger. Every minute counts, so let’s explore how to recognize a stroke and why rapid action is critical.
What a stroke is (short)
A stroke happens when the blood supply to part of the brain is suddenly interrupted or reduced. This prevents brain tissue from getting the oxygen and nutrients it needs, causing brain cells to start dying within minutes. There are two main types of stroke:
- Ischaemic stroke: This is the most common type. It is caused by a blockage (such as a blood clot) in an artery supplying blood to the brain.
- Haemorrhagic stroke: This occurs when a blood vessel in the brain bursts, causing bleeding into the surrounding tissue.
Both types are serious and require immediate medical attention. Without prompt treatment, a stroke can lead to lasting brain damage, disability, or death.
The FAST warning signs
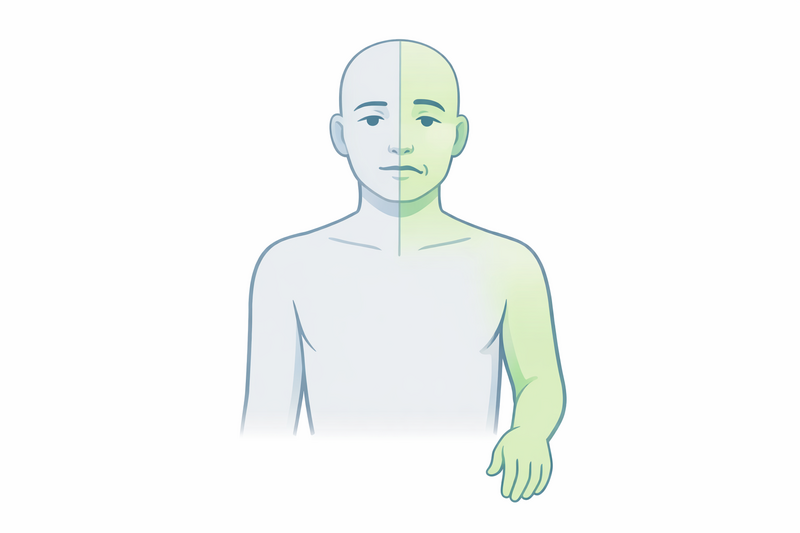
The FAST acronym is an easy way to remember the main warning signs of a stroke. These symptoms usually appear suddenly and are easy to recognise if you know what to look for. FAST stands for:
- F – Face: Has the person’s face dropped on one side? Can they smile? Often, a stroke will cause weakness or numbness on one side of the face, and the mouth or eye may droop.
- A – Arms: Can the person raise both arms and keep them there? After a stroke, there may be weakness or numbness in one arm, making it hard to lift or hold up.
- S – Speech: Is their speech slurred or unclear? Can they speak clearly and understand what you say? Speech problems are common in stroke, including difficulty finding words or speaking in full sentences.
- T – Time: If you notice any of these signs, it’s time to call emergency services immediately. The faster a person receives medical help, the better their chances of recovery.
Remember: Even if the symptoms disappear after a few minutes, it is still urgent to seek medical attention. These “mini-strokes” (also called transient ischaemic attacks, or TIAs) can be warning signs of a full stroke in the near future.
Other important stroke symptoms
While the FAST symptoms are the most common and widely recognised, strokes can also cause other warning signs. These may occur alone or together with FAST symptoms. Be alert for the following:
- Sudden vision problems: This can include blurred or double vision, or sudden loss of vision in one or both eyes.
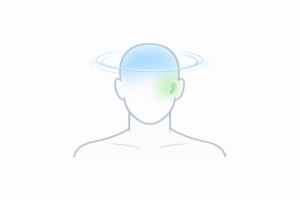
- Sudden severe headache: Especially if it is the worst headache you’ve ever had, and there is no obvious cause. This is more typical of haemorrhagic strokes.
- Sudden confusion or trouble understanding: The person may appear confused, have trouble following simple instructions, or seem disoriented.
- Sudden loss of balance or coordination: Difficulty walking, dizziness, or a sudden loss of balance may indicate a stroke, particularly if it comes on quickly and with no obvious reason.
- Sudden numbness or weakness: This may affect the leg on one side of the body, or sometimes both arms and/or legs.
- Trouble swallowing (dysphagia): Difficulty swallowing or choking on food or drink can be a sign.
Strokes can look different from person to person, and not everyone will have all of these symptoms. If you notice any sudden and unexplained changes in someone’s ability to move, speak, see, or understand, it’s better to be cautious and seek help immediately.
What to do immediately
If you suspect that someone is having a stroke, it is critical to act fast. Here are the steps you should take:
- Call emergency services straight away: Do not wait to see if the symptoms improve or go away. In most European countries, you can call 112 for emergency medical help.
- Note the time: Try to remember or write down when the symptoms began, or when the person was last seen well. This information is vital for doctors to determine the best treatment.
- Stay with the person: Keep them calm and comfortable. Do not give them anything to eat or drink, as swallowing may be affected.
- Do not attempt to drive them to the hospital yourself: Paramedics can provide life-saving care on the way and ensure the person gets to the right hospital quickly.
Some people may want to “wait and see” if the symptoms go away, but this can be very dangerous. Treatments for stroke are most effective when given as soon as possible after symptoms begin—ideally within the first few hours.
If you are alone and think you may be having a stroke, call emergency services immediately, unlock your door if you are able, and try to stay on the phone with the operator until help arrives.
What not to do
- Do not let the person fall asleep or “sleep it off.”
- Do not give them aspirin unless a doctor specifically says it is safe (it can be dangerous in some types of stroke).
- Do not give them food, water, or medication by mouth unless instructed by a healthcare professional.
When in doubt, always err on the side of caution—call for help at the first sign of a possible stroke.
What happens in the hospital
Once the person arrives at the hospital, a specialised team will act quickly to assess and treat the stroke. Here’s what usually happens:
- Immediate assessment: Doctors will check vital signs, ask about symptoms, and perform a quick physical and neurological examination.
- Brain imaging: A CT or MRI scan is used to determine what type of stroke has occurred (ischaemic or haemorrhagic) and where in the brain it is happening. This is essential, as treatments differ depending on the type.
- Possible treatments:
- For ischaemic stroke: If the person arrives within a certain time window (usually within 4.5 hours of symptom onset), they may receive a medication called a thrombolytic, which can dissolve the clot and restore blood flow.
- For haemorrhagic stroke: Treatment focuses on controlling bleeding and reducing pressure in the brain. This may involve medication, surgery, or other interventions.
- Monitoring and supportive care: The person will be closely monitored, with efforts to maintain normal blood pressure, blood sugar, and oxygen levels. Complications such as infection, deep vein thrombosis, or swallowing difficulties will be managed.
- Rehabilitation: Recovery from a stroke often involves rehabilitation to help the person regain lost skills and adapt to any lasting changes. This may include physiotherapy, occupational therapy, speech therapy, and support from a rehabilitation team.
The specific care and treatments will depend on the type, location, and severity of the stroke, as well as the person’s overall health.
It is common for families to feel overwhelmed after a loved one has a stroke. Hospital teams can provide information about the stroke, what to expect during recovery, and the support services available. Don’t hesitate to ask questions or voice any concerns you may have.
What happens after leaving the hospital?
Many people need ongoing rehabilitation and support after leaving the hospital. This can include:
- Regular physiotherapy and exercises to help improve movement and strength
- Speech and language therapy if communication or swallowing is affected
- Occupational therapy to adapt to daily routines
- Medication to reduce the risk of another stroke (such as blood thinners or blood pressure medicines)
- Emotional and psychological support, as stroke recovery can be challenging for both patients and families
Full recovery is possible for some people, but others may experience lasting effects. The earlier stroke is recognised and treated, the better the chances of a good outcome.
Because high blood pressure is one of the leading risk factors for stroke, it is important to learn about symptoms that often go unnoticed; you can find more details in our guide to the silent signs of high blood pressure you should not ignore.
When to see a doctor
If you or someone you know experiences any sudden changes in movement, speech, vision, or understanding—even if the symptoms improve quickly—it is essential to seek medical attention immediately. Early treatment can be life-saving and reduce the risk of long-term disability.
For anyone who has had a stroke or a TIA (mini-stroke), follow-up care with a doctor is crucial to manage risk factors and prevent another stroke. Speak to your GP or a specialist if you have concerns about your risk or need advice on lifestyle changes to reduce your chances of having a stroke.
Remember, knowing the signs and acting FAST can make all the difference. When it comes to stroke, every minute matters—your quick response could save a life.