If you experience headaches, you are certainly not alone. Head pain is a common complaint, but not all headaches are the same. Two of the most common types are migraines and tension headaches. Understanding the differences between these conditions can help you manage your symptoms more effectively and know when to seek medical advice. This article will guide you through the typical patterns, possible triggers, key symptoms, safe ways to manage headaches, and when it’s important to consult a doctor.
Typical pattern of each
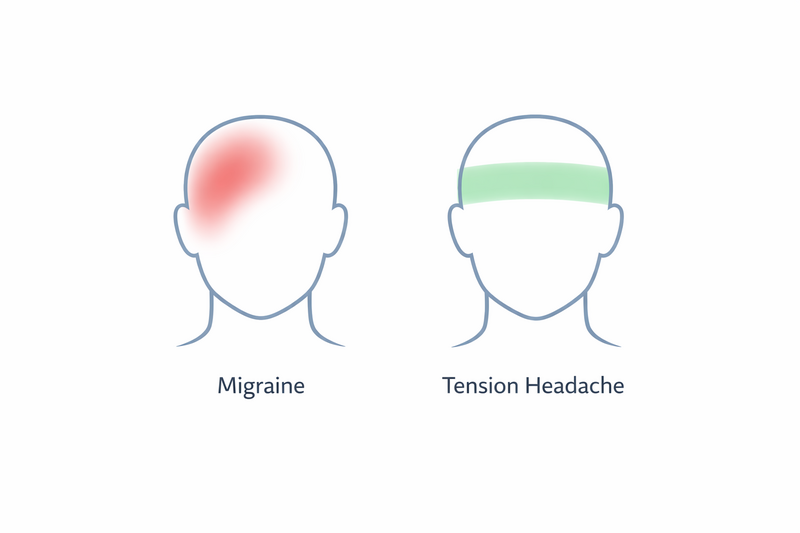
Migraines and tension headaches follow distinct patterns, which can help you identify which type you may be experiencing.
Migraine pattern
- Migraines often come in episodes, lasting from several hours up to three days.
- The pain usually affects one side of the head, but it can also shift or involve both sides.
- Headache pain is often moderate to severe and can worsen with routine physical activity.
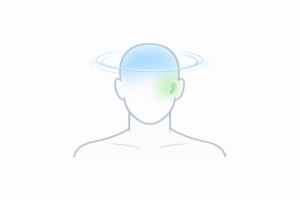
- Some people experience warning signs before a migraine, such as visual changes (called aura), sensitivity to light, or mood changes.
- Migraines may be accompanied by nausea or vomiting.
Tension headache pattern
- Tension headaches are often described as a constant, dull pain or pressure around the head, often like a tight band.
- The pain is usually mild to moderate and felt on both sides of the head.
- These headaches can last from 30 minutes to several days, but they are usually less severe than migraines.
- There are typically no warning signs or changes in vision before a tension headache starts.
- Physical activity does not usually make a tension headache worse.
Triggers and risk factors
Both migraines and tension headaches can be triggered by various factors, but their triggers are not always the same. Recognising your own triggers may help in managing headache episodes.
Common migraine triggers
- Hormonal changes, such as those related to the menstrual cycle
- Stress or emotional upsets
- Certain foods and drinks, including aged cheese, chocolate, caffeine, or alcohol
- Lack of sleep or changes in sleep patterns
- Bright lights, loud noises, or strong smells
- Skipping meals or dehydration
- Weather changes
Common tension headache triggers
- Prolonged stress or anxiety
- Poor posture, often related to long periods at a desk or computer
- Fatigue or lack of sleep
- Skipping meals
- Jaw clenching or teeth grinding
- Muscle tension in the neck, shoulders, or scalp
While both types of headaches can be linked to stress and tiredness, migraines are more likely to be triggered by specific foods or sensory stimuli, while tension headaches often relate to muscle tension and posture.
Key symptoms that differentiate them
Although migraines and tension headaches share some features, certain symptoms can help distinguish between the two.
How migraines feel
- Pain is often throbbing or pulsating
- Located on one side of the head (but can affect both sides)
- Moderate to severe intensity
- Worsens with physical activity
- May be accompanied by nausea, vomiting, or sensitivity to light and sound
- Some people experience aura: visual disturbances, tingling, or difficulty speaking before the headache starts
How tension headaches feel
- Pain is typically pressing or tightening, not throbbing
- Usually affects both sides of the head equally
- Mild to moderate intensity
- Does not worsen with routine activity
- No nausea or vomiting (though mild sensitivity to light or noise may occur)
- No aura or neurological symptoms
If your headache is severe, comes with neurological symptoms (such as visual changes, weakness, or speech problems), or lasts for several days, it is important to seek medical advice.
What helps (safe first steps)
For both migraines and tension headaches, there are some safe steps you can try at home. However, everyone is different, and what helps one person may not work for another. If in doubt, consult a healthcare professional before starting any new approach.
General tips for headache relief
- Rest in a quiet, dark room
- Apply a cold or warm compress to your forehead or neck
- Stay well hydrated
- Try gentle neck and shoulder stretches, especially for tension headaches
- Practice relaxation techniques such as deep breathing or mindfulness
- If you suspect a trigger (e.g., certain foods, poor posture), try to avoid it when possible
Over-the-counter medicines
- Paracetamol or ibuprofen may help relieve pain for both types of headache
- Avoid taking pain relievers more than two or three times a week to prevent medication-overuse headaches
- Do not mix medicines without checking with a pharmacist or doctor
For migraines, some people find relief with medicines specifically for migraines, such as triptans. These should only be used on advice from a healthcare professional.
Keeping a headache diary, noting when headaches occur, their severity, and possible triggers, can help you and your doctor find patterns and the best management approach.
When to see a doctor
Most headaches are not a sign of something serious, but certain features mean you should seek medical advice. It’s important to see a doctor if:
- Your headaches are frequent or severe, or interfere with daily life
- You need to take pain relievers for headaches more than twice a week
- You notice changes in your headache pattern, or new symptoms develop
- You have headaches along with fever, neck stiffness, rash, confusion, or weakness (these may suggest a more serious condition)
- Your headaches started after a head injury
- You are over 50 and have new or different headaches
A healthcare professional can help diagnose the type of headache you have, rule out other causes, and recommend safe and effective treatment options. In some cases, further investigations may be needed.
If you ever experience a sudden and extremely severe headache, it’s important to be aware of when this could signal an emergency—learn more about warning signs by reading when a sudden severe headache should be treated as an emergency.
In summary: Migraine and tension headaches are two of the most common headache types, but they have different typical patterns, triggers, and symptoms. Understanding these differences can help you manage your symptoms and know when to seek further help. If you have any doubts or if your headaches are affecting your quality of life, don’t hesitate to consult a healthcare professional for advice.