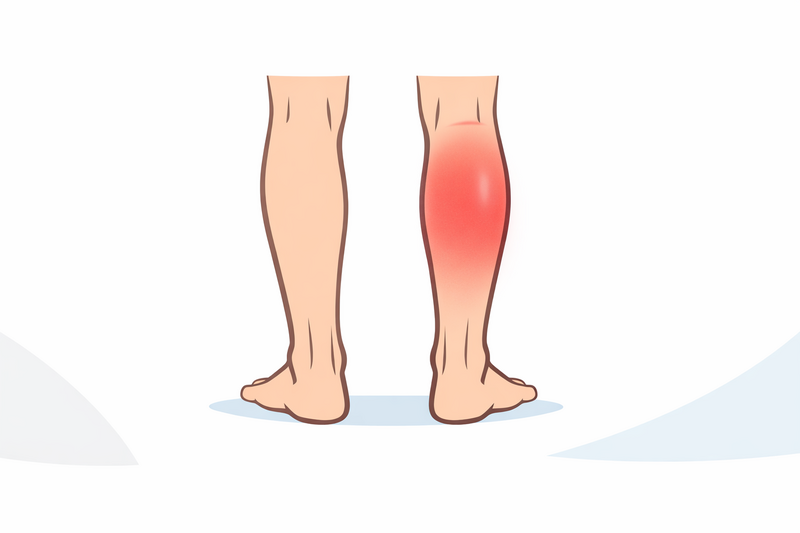
Leg swelling and calf pain are symptoms many people experience at some point in life. These symptoms are often due to harmless causes, such as muscle strain or standing for long periods. However, in some cases, they may point to a more serious underlying problem: a blood clot in the deep veins of the leg, known as deep vein thrombosis (DVT). Recognising when leg swelling and pain could be due to a DVT is crucial, as this condition can lead to life-threatening complications if not treated promptly.
This article will help you understand what DVT is, how to spot symptoms that may suggest a clot, and what to do if you are concerned. We will also cover emergency warning signs, what not to do, and how DVT is diagnosed and treated.
What a DVT is and why it matters
Deep vein thrombosis (DVT) is a condition where a blood clot forms in a deep vein, most commonly in the lower leg, thigh, or pelvis. Veins carry blood back to the heart, and when a clot blocks this flow, it can cause pain and swelling in the affected limb.
The main danger of a DVT is that part of the clot can break off and travel through your bloodstream to your lungs. This is called a pulmonary embolism (PE) and can be life-threatening, as it blocks blood flow to the lungs. For this reason, a DVT is a medical condition that should never be ignored or self-managed without medical advice.
- DVT most often affects the legs, but clots can form in other deep veins.
- Anyone can develop a DVT, but certain factors increase the risk (see below).
- Prompt recognition and treatment can prevent complications.
Understanding when to suspect a DVT can help you act quickly and avoid dangerous consequences.
Symptoms that make a clot more likely vs common causes
Not all leg pain or swelling is due to a blood clot. There are many common causes, such as:
- Muscle strains or sprains
- Minor injuries and bruises
- Long periods of standing or sitting
- Varicose veins
- Infections (cellulitis)
However, certain symptoms and risk factors make a DVT more likely. You should be especially alert if you notice:
- Swelling in one leg (rarely both), especially if it came on suddenly
- Pain or tenderness in the calf or thigh, often described as a cramp or ache
- Warmth or redness over the swollen or painful area
- Skin that looks pale, bluish, or reddish
- Swelling that does not improve with rest or elevation
Some people are at higher risk of developing DVT. Risk factors include:
- Recent surgery or hospital stay, especially involving the pelvis, hip, or leg
- Long periods of immobility (such as long-haul flights or car journeys)
- History of blood clots or clotting disorders
- Active cancer or recent cancer treatment
- Pregnancy or the first six weeks after giving birth
- Hormone therapy (such as certain birth control pills or HRT)
- Obesity
- Smoking
- Older age (risk increases especially after age 60)
If you have any of these risk factors and develop new, unexplained swelling and pain in your leg, it is important to seek medical advice as soon as possible.
Emergency warning signs of pulmonary embolism
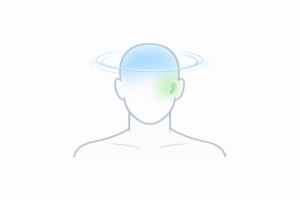
A DVT can become a medical emergency if part of the clot travels to the lungs, causing a pulmonary embolism (PE). This is a life-threatening situation that requires immediate medical attention. Call emergency services right away if you experience:
- Sudden shortness of breath for no obvious reason
- Sharp chest pain or discomfort, which may get worse when you breathe in deeply
- Rapid heartbeat or palpitations
- Coughing up blood
- Feeling dizzy, faint, or lightheaded
These symptoms can develop quickly and may be accompanied by anxiety or a sense of impending doom. Do not attempt to drive yourself to the hospital—instead, call emergency services immediately if you suspect a pulmonary embolism.
What to do now (and what to avoid)
If you think you might have a DVT (for example, you have new, unexplained leg swelling and pain, especially with risk factors):
- Contact a doctor or go to an urgent care centre without delay.
- If advised to go to hospital, do not walk or exert yourself more than necessary, as activity could dislodge a clot.
- Do not attempt to treat the symptoms yourself with home remedies or over-the-counter painkillers.
- Do not massage the leg—this could increase the risk of the clot moving.
- Keep your leg raised and rest while you wait for medical assessment, unless told otherwise by a healthcare professional.
Prompt assessment and treatment can significantly reduce your risk of complications. If you are in doubt, it is always safer to seek medical advice and rule out a serious cause.
When is it safe to wait?
Most cases of sudden leg swelling and pain should be checked by a doctor, especially with risk factors for DVT. If your symptoms are mild, have a clear explanation (such as a recent injury), and improve with rest, you may monitor them. However, if in doubt, err on the side of caution and consult a healthcare provider.
How DVT is diagnosed and treated
If a doctor suspects you have DVT, they will assess your symptoms, medical history, and risk factors. Diagnosis is usually confirmed with imaging tests, such as:
- Ultrasound scan: The most common and non-invasive test for detecting clots in the leg veins.
- Blood tests (D-dimer): Can help rule out a clot if the result is normal and suspicion is low.
- Other imaging: In rare cases, further tests such as CT or MRI scans may be needed.
If a DVT is confirmed, treatment aims to stop the clot from growing, prevent it from moving to the lungs, and reduce the chance of future clots. The main treatments are:
- Anticoagulant medicines (blood thinners): These do not dissolve existing clots but prevent them from getting bigger and new ones from forming. Treatment usually lasts for at least three months.
- Compression stockings: May be recommended to reduce swelling and lower the risk of long-term complications, such as post-thrombotic syndrome.
- Monitoring and follow-up: Regular check-ups to assess your response to treatment and adjust medication as needed.
- Hospital admission: Some people may need to stay in hospital, especially if they have a large clot, are at high risk of complications, or cannot take blood thinners.
In rare cases, procedures to remove the clot or insert a filter in a large vein (inferior vena cava filter) may be considered, usually for people who cannot take blood thinners or have had a serious complication.
Most people recover fully from a DVT with proper treatment, but it is important to take medicines exactly as prescribed and attend all follow-up appointments. Your doctor will advise you on activity, travel, and how to reduce the risk of another clot in the future.
Prevention tips for those at risk
If you are at increased risk of DVT, your healthcare provider may recommend:
- Staying active and moving regularly, especially on long journeys
- Wearing compression stockings if advised
- Drinking plenty of fluids (unless told otherwise)
- Managing weight and avoiding smoking
- Discussing risk factors before planned surgery or hospital admission
If you have a history of DVT or are on blood thinners, talk to your doctor before starting any new medication or making significant lifestyle changes.
If you are experiencing symptoms such as sudden shortness of breath and want to learn which warning signs should never be ignored, our guide on serious causes of shortness of breath and red flag symptoms offers further advice.
In summary: Leg swelling and calf pain can have many causes, but a blood clot (DVT) is a serious condition that needs urgent attention. If you have symptoms or risk factors for DVT, seek prompt medical advice. Recognising the warning signs and acting quickly can protect your health and potentially save your life.
If you are ever unsure, it is always better to speak to a healthcare professional for guidance.