Fatty liver disease is a common but often overlooked condition affecting millions of people across Europe and the world. Many people with fatty liver disease do not realise they have it, as the symptoms can be very subtle or even absent for years. Understanding what fatty liver disease is, how it develops, and why it is frequently missed is important for anyone interested in protecting their liver health.
This article explains what fatty liver disease means, why its symptoms are so easy to overlook, how doctors detect it, and when lifestyle changes can make a difference. If you are concerned about your liver health or have risk factors such as being overweight, having diabetes, or drinking alcohol regularly, learning about fatty liver disease can help you make informed decisions and seek appropriate advice from your healthcare provider.
What fatty liver disease means
Fatty liver disease refers to the build-up of excess fat in the cells of the liver. The liver is a vital organ responsible for many important functions, including filtering toxins, storing nutrients, and helping with digestion. When too much fat accumulates in the liver, it can interfere with these processes and eventually lead to more serious health problems.
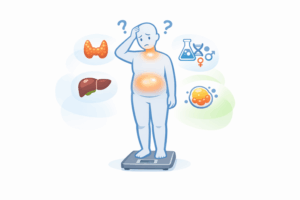
There are two main types of fatty liver disease:
- Non-alcoholic fatty liver disease (NAFLD): This is the most common form, especially in Europe. It occurs in people who drink little or no alcohol, and is often related to being overweight, having high cholesterol, type 2 diabetes, or high blood pressure.
- Alcohol-related fatty liver disease (ARLD): This type is caused by drinking more alcohol than the liver can safely process, leading to fat build-up and, eventually, liver damage.
Both types of fatty liver disease can progress through several stages:
- Simple fatty liver (steatosis): Fat accumulates in the liver but causes little or no inflammation or damage in the early stages.
- Steatohepatitis: As the disease advances, the liver may become inflamed (non-alcoholic steatohepatitis, NASH, or alcoholic steatohepatitis, ASH), which increases the risk of scarring.
- Fibrosis and cirrhosis: Ongoing inflammation can lead to scarring (fibrosis) and, eventually, severe scarring (cirrhosis), which can cause the liver to stop working properly.
It is important to note that not everyone with fatty liver disease will progress to these more serious stages, but the risk increases if the underlying causes are not addressed.
Why symptoms are subtle
One of the main reasons fatty liver disease is often missed is that it tends to develop slowly and silently. Most people with early-stage fatty liver disease experience no obvious symptoms. Even as the condition progresses, symptoms can be vague and easily attributed to other causes.
Common reasons why symptoms are subtle or absent include:
- Gradual development: Fat accumulates in the liver over many years, giving the body time to adjust and compensate without noticeable signs.
- Lack of nerve endings: The liver has very few nerve endings, so damage or inflammation rarely causes pain until the disease is advanced.
- Non-specific symptoms: If symptoms do occur, they may include tiredness, mild discomfort in the upper right abdomen, or feeling generally unwell—symptoms that can be caused by many other conditions.
Because of this, fatty liver disease is often discovered only incidentally—such as during a routine blood test or an ultrasound scan for another reason. By the time symptoms become more obvious, such as jaundice (yellowing of the skin or eyes), swelling, or confusion, the disease may already be quite advanced.
It is important to remember that having risk factors (like obesity, type 2 diabetes, high blood pressure, or regular alcohol consumption) increases the chances of developing fatty liver disease, even if you feel perfectly healthy.
How it’s detected
Since fatty liver disease often causes few or no symptoms, it is usually detected through routine medical tests or investigations for other health concerns. There is no single test that can definitively diagnose all forms of fatty liver disease, so doctors use a combination of methods to assess liver health and rule out other causes.
Blood tests
Doctors may order blood tests to check for signs of liver inflammation or damage. These include liver function tests (ALT, AST, and others). However, blood tests alone cannot confirm fatty liver disease, as results may be normal even when fat is present in the liver.
Imaging tests
Ultrasound scans are often used to look at the liver. An ultrasound can show if the liver appears enlarged or if there is excess fat. Sometimes, other imaging techniques such as CT scans or MRI scans may be used for more detail.
Fibroscan and other specialised tests
In some cases, a Fibroscan (transient elastography) is used to measure liver stiffness. This test can help detect scarring (fibrosis) and assess how advanced the disease may be.
Liver biopsy
Rarely, a small sample of liver tissue may be taken (biopsy) to confirm the diagnosis and check for inflammation or scarring. This is usually only done if the diagnosis is unclear or if advanced disease is suspected.
Doctors may also ask about your medical history, alcohol intake, body weight, and other risk factors to help determine the most likely cause of liver changes.
Importantly, early detection gives the best chance of preventing progression to more serious liver problems. If you are at higher risk, your doctor may recommend regular monitoring even if you feel well.
When lifestyle changes are advised
For most people with fatty liver disease, making certain lifestyle changes is the main way to manage the condition and prevent it from getting worse. Unlike some other diseases, there is no specific medication approved to “cure” fatty liver disease. However, positive changes can significantly improve liver health and overall wellbeing.
Doctors may recommend lifestyle changes if:
- You are overweight or obese
- You have type 2 diabetes, high cholesterol, or high blood pressure
- You drink more alcohol than recommended
- Blood tests or scans show evidence of fatty liver, even if you have no symptoms
Key lifestyle changes that may help
- Healthy weight loss: Gradually losing 5–10% of your body weight can reduce fat in the liver and may even reverse early-stage disease.
- Balanced diet: Eating more fruit, vegetables, whole grains, and healthy fats (such as those in olive oil and nuts), while reducing added sugars, processed foods, and saturated fats, is beneficial.
- Regular physical activity: Moderate exercise, such as brisk walking, cycling, or swimming, for at least 150 minutes per week is recommended.
- Limiting alcohol: Reducing or avoiding alcohol can prevent further liver damage, especially in people with alcohol-related fatty liver disease.
- Managing other health conditions: Keeping diabetes, high blood pressure, and high cholesterol under good control helps protect the liver.
These changes may seem challenging at first, but even small, sustained improvements can make a big difference. Support from healthcare professionals, dietitians, or patient groups can be very helpful if you are unsure where to start.
In more advanced cases, or if lifestyle changes are not enough, a doctor may discuss other treatments or refer you to a liver specialist (hepatologist).
If you are interested in learning more about how ultrasound scans are used to detect liver changes, including their benefits and limitations, you can read our detailed guide on what ultrasound can and cannot show for liver health.
Fatty liver disease is common and often silent, but it is not inevitable. With greater awareness, regular health checks, and healthy lifestyle choices, most people can prevent serious complications and maintain good liver health. If you have concerns about your liver or risk factors for fatty liver disease, speak to your doctor for personalised advice and support.