Colon cancer is one of the most common cancers in Europe, but its early symptoms can be easy to overlook. Many people dismiss the initial signs as minor health issues or natural changes in their bodies. Understanding these symptoms, and knowing when to seek medical advice, can make a significant difference in early detection and treatment outcomes.
This article explores why early symptoms of colon cancer are often subtle, which signs people tend to ignore, and what risk factors and diagnostic tests are important for patients to know about.
Why early symptoms are subtle
Colon cancer develops in the large intestine, often starting as small, noncancerous growths called polyps. These polyps typically do not cause any discomfort or noticeable symptoms at first. As a result, colon cancer can progress quietly for months or even years before more obvious health problems arise.
There are several reasons why the early symptoms of colon cancer may be overlooked:
- Slow development: Colon cancer tends to grow slowly, so symptoms may be mild or come and go.
- Non-specific symptoms: Early signs are often similar to common digestive issues, such as bloating, mild cramps, or changes in bowel habits.
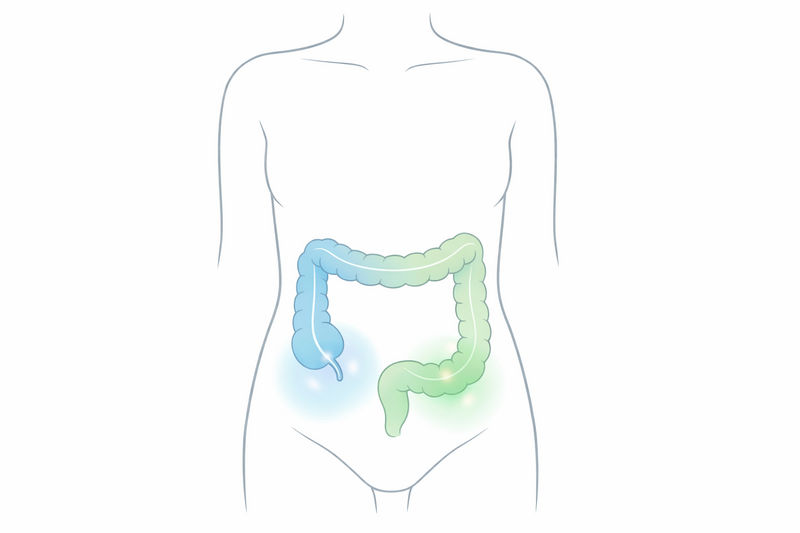
- Location matters: The exact symptoms can depend on where in the colon the cancer starts. Tumours on the right side (ascending colon) may cause different symptoms than those on the left (descending colon).
- Body adapts: The colon can sometimes compensate for changes caused by a tumour, masking symptoms until the cancer is more advanced.
Because the signs can be so mild, it is easy to attribute them to factors like diet, stress, or ageing. This is why awareness and regular screening are crucial, especially for those at higher risk.
Symptoms people normalize
Many early symptoms of colon cancer overlap with everyday complaints, which can lead to them being dismissed or normalized. Some of the most common signs include:
- Changes in bowel habits: This could mean more frequent or less frequent bowel movements, persistent constipation, or diarrhea that lasts for more than a few days.
- Blood in the stool: Blood may appear bright red or darker, and sometimes it is not visible to the naked eye. It is often mistaken for hemorrhoids or minor tears.
- Unexplained fatigue: Ongoing tiredness without a clear reason may be linked to slow blood loss from the colon, leading to anemia.
- Abdominal discomfort: Mild cramps, bloating, feeling of fullness, or gas pains are easily attributed to diet or stress.
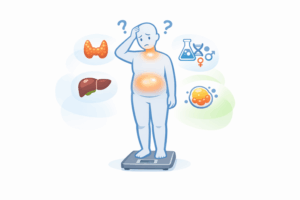
- Unintentional weight loss: Losing weight without trying can be a warning sign, but it is often overlooked or considered a positive change.
- Incomplete emptying: A persistent sensation that the bowel does not empty completely after a movement.
It is important to remember that these symptoms do not always mean colon cancer. They can be caused by many other, less serious conditions. However, if they persist or are unusual for your body, it is best to consult a healthcare professional.
Risk factors that raise concern
While colon cancer can affect anyone, certain factors increase the risk of developing the disease. Understanding these risks can help people decide when to be more vigilant and proactive about symptoms.
- Age: Most cases occur in people over 50, but younger adults can also be affected.
- Family history: Having a parent, sibling, or child with colon cancer or polyps increases your risk.
- Personal history: If you have had colon polyps or inflammatory bowel diseases like Crohn’s disease or ulcerative colitis, your risk is higher.
- Lifestyle factors: Diets high in processed meats and low in fiber, sedentary lifestyle, obesity, smoking, and heavy alcohol use all contribute to increased risk.
- Genetic syndromes: Certain inherited conditions, such as Lynch syndrome or familial adenomatous polyposis (FAP), greatly increase the risk.
If you have any of these risk factors, it is important to discuss screening options and symptom monitoring with your doctor, even if you feel healthy.
When to seek assessment
Knowing when to consult a doctor can be difficult, especially when symptoms are mild or variable. However, there are certain signs and situations in which medical assessment should not be delayed:
- Persistent changes: Any new or ongoing changes in bowel habits that last more than three weeks.
- Visible blood: Noticing blood in or on your stool, especially if it happens more than once.
- Unexplained symptoms: Ongoing fatigue, weight loss, or abdominal discomfort without another clear cause.
- Family or personal risk: If you have a strong family history or previous colon problems, even mild symptoms should be discussed with a healthcare provider.
Your doctor will ask about your symptoms, medical history, and may perform a physical examination. Based on this information, they may recommend further tests to determine the cause of your symptoms.
It is always better to check with a healthcare professional if you are concerned. Early assessment can help identify colon cancer or other conditions when they are easiest to manage.
What tests are commonly used
If your doctor suspects colon cancer or wants to rule it out, several tests may be used to investigate further. The choice of test depends on your symptoms, medical history, and risk factors.
- Fecal occult blood test (FOBT): This simple test checks for hidden (occult) blood in the stool, which can be a sign of bleeding from a tumor or polyp.
- Fecal immunochemical test (FIT): Similar to FOBT, FIT looks for blood in the stool using antibodies, and does not require dietary restrictions before the test.
- Colonoscopy: A thin, flexible tube with a camera is used to examine the entire colon. It allows doctors to find and remove polyps, and take biopsies of suspicious areas.
- Flexible sigmoidoscopy: Like a colonoscopy, but only examines the lower part of the colon. It may be used for initial screening or when symptoms suggest an issue in this area.
- CT colonography (virtual colonoscopy): This imaging test uses CT scans to produce detailed pictures of the colon and rectum. It is less invasive but may require a follow-up colonoscopy if abnormalities are found.
- Blood tests: While blood tests alone cannot diagnose colon cancer, they may show signs of anemia or help assess overall health.
Screening tests are often recommended for people aged 50 and above, or earlier for those with increased risk. Early detection through screening can find polyps before they turn into cancer, or catch cancer at a curable stage.
If a test finds an abnormality, further procedures such as biopsies or scans may be needed to confirm the diagnosis and plan treatment. Your healthcare team will explain each step and answer any questions you may have.
If you are concerned about noticing blood in your stool or want to understand what different causes might mean, you can find more information in our guide to common causes of blood in stool and when to seek help.
In summary: Colon cancer can be difficult to detect early because its symptoms are subtle and easily mistaken for less serious problems. If you notice persistent changes in your bowel habits, blood in your stool, unexplained fatigue, or other unusual symptoms, especially if you have risk factors, do not hesitate to seek medical advice. Early assessment and appropriate testing can make a significant difference in outcomes. Regular screening is the best way for many people to stay ahead of this disease.