Breathing difficulties are a common cause of concern for many people. If you have ever found yourself short of breath, with tightness in your chest, or feeling as if you can’t get enough air, you may have wondered: is this asthma, or is it anxiety? The answer isn’t always straightforward, because the symptoms of asthma and anxiety can overlap in surprising ways. Understanding the differences—and what to do when you’re not sure—can help you feel more in control and know when to seek medical advice.
This article explains why asthma and anxiety can both cause troubling breathing symptoms, how you can spot clues that point to one or the other, and what steps to take if you’re worried about your health. Remember, when in doubt, it’s always best to speak to a healthcare professional.
How asthma and anxiety can overlap
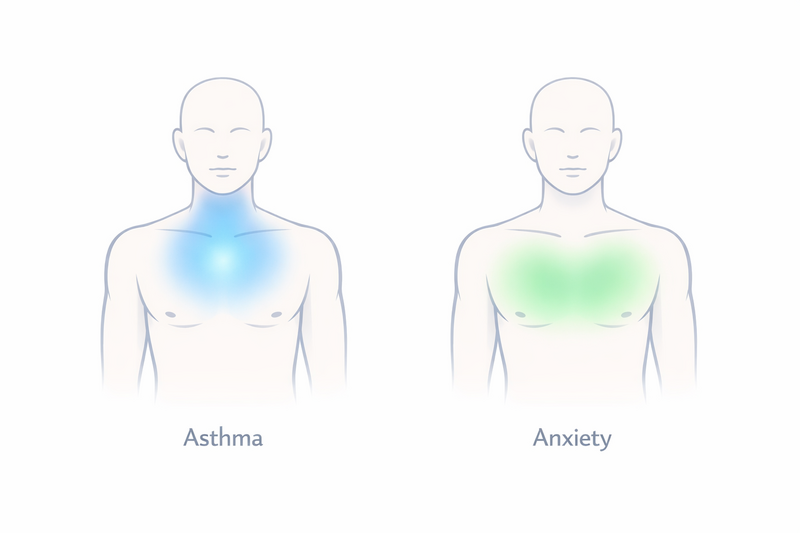
Asthma and anxiety are very different conditions, but they can produce similar sensations, especially when it comes to breathing. Asthma is a physical condition that affects the airways in your lungs, while anxiety is a mental health condition that can cause physical symptoms due to the body’s stress response. Here’s why the overlap happens:
- Shortness of breath: Both asthma and anxiety can make you feel like you can’t get enough air.
- Chest tightness: Tightness or pressure in the chest occurs in both conditions, though for different reasons.
- Rapid breathing: Anxiety can lead to hyperventilation (breathing too quickly), while asthma can make you breathe faster as your body tries to get more oxygen.
- Coughing: Some people with anxiety cough or clear their throat, while coughing is also a common asthma symptom.
The body’s response to stress and fear includes physical changes—like faster heartbeat, sweating, and rapid breathing—that can feel very similar to the symptoms caused by asthma. In some cases, anxiety can even trigger an asthma attack in people who already have asthma. This overlap can make it hard to tell which condition is responsible for your symptoms, especially if you live with both asthma and anxiety.
Clues that point to asthma
Asthma is a chronic condition where the airways become inflamed and narrowed, making it difficult to breathe. Certain clues can help you recognise when your symptoms are more likely to be caused by asthma:
- Wheezing: A whistling or squeaky sound when you breathe out is very typical of asthma, though not everyone with asthma will have this symptom.
- Symptoms triggered by allergens or irritants: Symptoms often get worse around dust, pollen, smoke, pets, cold air, or after exercise.
- Night-time symptoms: Asthma often disturbs sleep, making you wake up coughing or short of breath.
- Relief with inhalers: If you use a reliever inhaler (like salbutamol) and your symptoms improve quickly, asthma is likely to be the cause.
- History of allergies or eczema: People with asthma often have a personal or family history of allergies, hay fever, or eczema.
Asthma attacks can come on gradually or suddenly, and symptoms may be mild or severe. If you suspect asthma, especially if you have had symptoms for a long time or they worsen with certain triggers, it’s important to discuss this with your doctor. They may recommend tests like spirometry (which measures how well your lungs work) or a trial of asthma medication.
Clues that point to anxiety/panic
Anxiety and panic attacks can also cause intense breathing symptoms, often accompanied by other signs. Certain features may suggest anxiety or panic is the main problem:
- Sudden onset during stress: Symptoms often appear quickly in response to stressful situations or strong emotions.
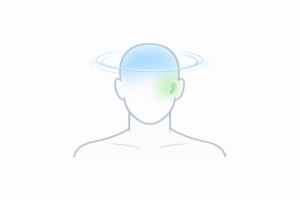
- Other anxiety signs: Trembling, sweating, racing heart, dizziness, nausea, or a sense of impending doom often accompany anxiety-related breathing difficulties.
- Sense of “air hunger”: People with anxiety often describe feeling like they can’t get a deep enough breath, even though their oxygen levels are normal.
- Symptoms improve with distraction or relaxation: Focusing on something else, breathing slowly, or calming techniques often help symptoms ease.
- No clear physical triggers: Symptoms do not reliably happen with exercise, allergens, or when exposed to cold air.
- Previous history of anxiety: A known diagnosis of anxiety or panic disorder, or a pattern of similar episodes in the past, can be a clue.
Panic attacks can be particularly frightening, with symptoms peaking within a few minutes and then improving. While these attacks can feel life-threatening, they are not usually dangerous in themselves. However, it’s important to see a healthcare professional to rule out other causes—especially if you’re unsure or if it’s your first episode.
When symptoms are an emergency
Whether you have asthma, anxiety, or are unsure of the cause, certain breathing symptoms require urgent medical attention. Knowing when to act quickly can be life-saving. Seek emergency help if you experience:
- Severe shortness of breath, making it hard to speak or walk
- Lips, face, or fingers turning blue or grey
- Feeling faint, dizzy, or confused
- Chest pain that does not go away
- No improvement after using your reliever inhaler (if you have one)
- Symptoms that come on very suddenly and do not improve with rest
If you have a known asthma diagnosis and your symptoms are worsening quickly, follow your asthma action plan if you have one, and seek help if you do not improve. If you are experiencing a panic attack for the first time and are worried, it’s always better to get checked by a doctor or go to the emergency department. Never hesitate to seek urgent care if you are unsure—medical teams are trained to tell the difference and provide the right support.
How doctors sort it out
When you see a doctor about breathing problems, they will work with you to figure out the likely cause. This usually involves:
- Detailed history: The doctor will ask about your symptoms, what triggers them, how long they last, and what makes them better or worse.
- Physical examination: Listening to your lungs, checking your heart, and looking for other signs can provide important clues.
- Breathing tests: Tests like spirometry measure how well your lungs are working and can help diagnose asthma or other lung diseases.
- Response to treatment: Improvement with asthma medication suggests asthma; improvement with relaxation or anti-anxiety measures may suggest anxiety.
- Blood tests or imaging: Occasionally, further tests are done to rule out infections, heart problems, or other conditions.
Doctors are trained to look for “red flag” symptoms that suggest a more serious problem. In some cases, both asthma and anxiety may be present, and treating both can lead to the best outcome. If anxiety is diagnosed, your doctor may suggest talking therapies, lifestyle changes, or sometimes medication. For asthma, inhalers and avoiding triggers are common treatments. If you’re living with both conditions, managing stress and following your asthma plan are both important.
It’s helpful to keep a diary of your symptoms, noting when they happen, how long they last, and what you were doing at the time. This information can help your doctor make a diagnosis and tailor the right treatment for you.
If you are interested in learning more about warning signs, you may find our guide on important red flags for shortness of breath helpful for understanding when to seek urgent care.
In summary, while asthma and anxiety are very different, they can both cause breathlessness and chest symptoms that are hard to tell apart. If you’re ever unsure or if symptoms are severe, seek medical advice promptly. Your healthcare team can help you understand your symptoms, rule out serious causes, and find the best way forward for your health and peace of mind.