Abdominal pain is a common complaint that most people experience at some point in their lives. While many causes of abdominal pain are harmless and resolve on their own, some can signal a more serious underlying problem that needs urgent medical attention. Understanding the difference between common benign causes and red flags is important for knowing when to seek help and when you may be able to manage symptoms at home.
This article will guide you through the most frequent harmless reasons for abdominal pain, highlight warning signs you should never ignore, explain how the location and pattern of pain matters, and offer practical advice on safe home care. You’ll also learn what to expect if you visit a doctor about your abdominal pain, including common tests and evaluations.
Common benign causes of abdominal pain
Most episodes of abdominal pain are not caused by anything dangerous. Here are some of the most frequent benign causes:
- Indigestion (dyspepsia): Overeating, eating too quickly, consuming spicy or fatty foods, or drinking alcohol can all cause temporary discomfort in the upper abdomen. This is often described as a burning or aching sensation.
- Gastroenteritis (“stomach flu”): Viral or bacterial infections can irritate the stomach and intestines, leading to crampy pain, nausea, vomiting, and diarrhoea. Symptoms usually improve within a few days.
- Constipation: Difficulty passing stool can cause bloating, cramping, and discomfort, particularly in the lower abdomen. This is common in people who do not drink enough fluids or eat enough fibre.
- Menstrual cramps: Many women experience lower abdominal pain in the days before or during their period. This pain is typically due to the normal hormonal changes of the menstrual cycle.
- Gas and bloating: Swallowing air, certain foods, or digestive issues can lead to the build-up of gas in the intestines, causing sharp or crampy abdominal pain that often moves around.
- Muscle strain: Overexertion, exercise, or heavy lifting can cause soreness in the abdominal muscles, which may be mistaken for internal pain.
- Food intolerance: Some people experience abdominal discomfort after eating certain foods, such as lactose (in dairy products) or gluten (in wheat), due to difficulty digesting them.
These causes are generally self-limiting and do not require specific medical treatment. However, if pain is severe, persistent, or associated with other concerning symptoms, it is important not to dismiss it as harmless.
Red flags that need urgent care
While most abdominal pain is not serious, certain warning signs (“red flags”) may indicate a potentially dangerous condition. You should seek immediate medical attention if you experience any of the following:
- Sudden, severe pain: Especially if it comes on rapidly or is the worst pain you have ever felt.
- Pain with fever and vomiting: Particularly if accompanied by inability to keep fluids down or signs of dehydration.
- Blood in vomit or stool: Vomiting blood (which may look like coffee grounds) or passing black, tarry, or bloody stools can signal internal bleeding.
- Persistent pain with weight loss: Unexplained weight loss alongside ongoing abdominal discomfort should be investigated.
- Pain with difficulty breathing or chest pain: Sometimes, heart problems can cause pain in the upper abdomen or chest.
- Severe pain during pregnancy: Any significant abdominal pain in pregnancy, especially if associated with bleeding, should be checked immediately.
- Abdominal swelling or a rigid, tender abdomen: A hard, swollen, or painful abdomen that does not improve can be a sign of a serious problem.
- Persistent vomiting or inability to pass stool/gas: These can indicate a blockage in the bowel.
- Pain following recent abdominal injury: Trauma or injury to the abdomen can cause internal bleeding or organ damage.
These symptoms may be linked to conditions such as appendicitis, bowel obstruction, gallstones, pancreatitis, perforated ulcers, or even heart attack, and require prompt evaluation by a medical professional.
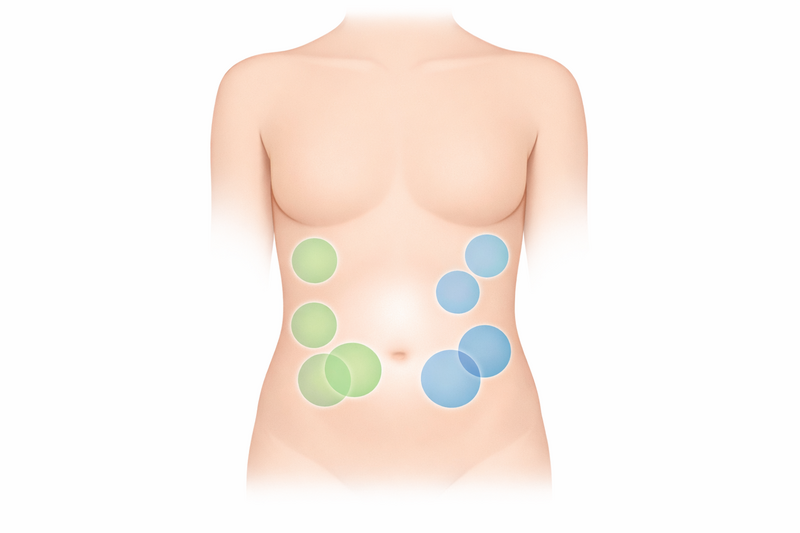
Where the pain is: patterns that help
The location and nature of abdominal pain can provide important clues about its cause. Here are some common patterns:
- Upper abdomen (epigastric pain): Often related to the stomach, oesophagus, or upper part of the small intestine. Common causes include indigestion, gastritis, or ulcers. Pain after eating fatty foods may be due to gallbladder issues.
- Lower right abdomen: Pain here, especially if worsening over time, can be a sign of appendicitis. However, it may also be caused by constipation or menstrual cramps.
- Lower left abdomen: Commonly linked to constipation or, in older adults, diverticulitis. In women, ovarian cysts or gynaecological issues may also cause pain in this area.
- Central abdominal pain: Often non-specific and may be related to gastroenteritis, irritable bowel syndrome (IBS), or early appendicitis.
- Upper right abdomen: Pain here may be due to gallstones, liver problems, or sometimes, referred pain from the lungs or heart.
- Generalised pain (all over): This can occur with viral infections (“stomach flu”), gas, or more serious conditions like peritonitis (inflammation of the abdominal lining).
- Pain that moves: For example, pain that starts in the centre and moves to the lower right side can be typical of appendicitis.
It can be useful to note exactly where your pain is, whether it moves, what makes it better or worse, and if it is constant or comes and goes. This information can help your doctor make a more accurate diagnosis.
What you can try safely at home (and what to avoid)
If you have mild abdominal pain without any red flags, there are several things you can do to relieve your discomfort:
- Rest and hydration: Take it easy and drink plenty of fluids, especially if you have diarrhoea or vomiting.
- Eat light, bland foods: Foods like bananas, rice, toast, and applesauce are gentle on the stomach and can help with mild nausea.
- Apply gentle heat: A warm (not hot) water bottle or heating pad on your abdomen may ease cramping or muscle soreness.
- Over-the-counter remedies: For minor pain, medicines like paracetamol can be used. Avoid nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, especially if you have stomach ulcers or gastritis, as these may worsen symptoms.
- Monitor your symptoms: Keep track of what makes your pain better or worse and any new symptoms that develop.
What to avoid:
- Do not take strong painkillers or medicines prescribed for someone else.
- Avoid alcohol and fatty or spicy foods until you are feeling better.
- Do not use laxatives for constipation unless recommended by a doctor, especially if you also have vomiting or severe pain.
- Avoid strenuous activity until your symptoms improve.
If your symptoms do not improve after a few days, or if you develop any red flags, contact your healthcare provider for further advice.
What doctors evaluate and common tests
If you visit a doctor with abdominal pain, they will start by asking about your symptoms in detail. You can expect questions about:
- When the pain started and how long it lasts
- Where the pain is located and whether it moves
- The type of pain (sharp, dull, crampy, constant or intermittent)
- What makes the pain better or worse
- Associated symptoms such as fever, vomiting, diarrhoea, constipation, weight loss, or urinary symptoms
- Your medical history, medications, recent travel, and family history of digestive diseases
After the initial discussion, the doctor will usually perform a physical examination, checking your abdomen for tenderness, swelling, or any masses. They may also listen for bowel sounds and check other vital signs such as blood pressure, heart rate, and temperature.
Depending on your symptoms and examination, the doctor may order one or more of the following tests:
- Blood tests: To look for signs of infection, inflammation, anaemia, or problems with organs like the liver and pancreas.
- Urine tests: To check for urinary tract infections or kidney problems.
- Stool tests: To look for infection, blood, or signs of malabsorption.
- Ultrasound scan: A painless imaging test often used to look at organs such as the liver, gallbladder, kidneys, and pelvic organs.
- X-rays or CT scans: More detailed imaging that can help identify blockages, inflammation, or complications like perforation.
- Endoscopy: In some cases, a flexible camera is used to look directly inside the stomach or intestines.
Most cases of mild, short-lived abdominal pain do not need extensive testing. However, if your doctor is concerned about a serious cause, or if pain does not improve, further investigation may be needed.
If you notice changes in your bowel movements, such as the presence of blood in your stool along with abdominal pain, it is important to read about common causes and warning signs of blood in stool so you know when to seek prompt medical advice.
Remember, abdominal pain can have many causes, and it is always better to err on the side of caution. If you are unsure or your symptoms worsen, contact a healthcare professional for advice.