Colonoscopy is an important medical procedure that allows doctors to examine the inside of your large intestine (colon and rectum). Many people feel anxious when their doctor recommends a colonoscopy, but understanding the process can help you feel more comfortable and prepared. In this article, we explain why colonoscopy is recommended, how to prepare, what happens during the procedure, and what to expect during recovery and when receiving your results.
Whether you are having a colonoscopy for the first time or returning for routine screening, knowing what to expect can help you approach the process with confidence and peace of mind.
Why colonoscopy is recommended
Your doctor may recommend a colonoscopy for several reasons. The main aim is to detect changes or abnormalities in the colon and rectum. Early detection of certain conditions can make a significant difference in treatment and outcomes.
- Screening for colorectal cancer: Colonoscopy is the gold standard for screening for colorectal cancer, especially in people over 50 or those with a family history of colorectal cancer.
- Investigating symptoms: If you have symptoms such as persistent abdominal pain, rectal bleeding, unexplained changes in bowel habits, or unexplained weight loss, a colonoscopy can help to identify the cause.
- Monitoring inflammatory bowel disease: For patients with conditions like Crohn’s disease or ulcerative colitis, colonoscopy is used to monitor the lining of the colon and assess disease activity.
- Surveillance after polyps or cancer: If you have had polyps removed or have been treated for colon cancer, regular colonoscopies are often recommended to check for recurrence or new growths.
Doctors also use colonoscopy to remove polyps (small growths that could develop into cancer) and to take tissue samples (biopsies) for further testing. By identifying problems early, colonoscopy can help prevent serious illness and guide your ongoing care.
Preparation steps
Preparing for a colonoscopy is a key part of ensuring the procedure is effective and accurate. The preparation process, often called “bowel prep,” aims to empty your colon of all solid matter so the doctor can see clearly during the examination.
Consultation with your doctor
Before your colonoscopy, you will have a discussion with your doctor or nurse. They will review your medical history, any medications you are taking, and any allergies you may have. It’s important to mention all medicines, including blood thinners, diabetes medication, or supplements, as you may need to adjust these before the procedure.
Dietary restrictions
In the days leading up to your colonoscopy, you may be asked to avoid certain foods, such as seeds, nuts, or high-fibre foods. Usually, you will be told to have only clear liquids (such as water, broth, tea, or clear juices) the day before your procedure. Avoid red or purple drinks, as they can be mistaken for blood during the exam.
Bowel cleansing
The most important part of preparation is taking a prescribed laxative to clean out your colon. This usually involves drinking a special solution the evening before (and sometimes the morning of) your colonoscopy, according to your doctor’s instructions. It is common to make several trips to the bathroom during this time as your body clears out the bowel.
- Follow the specific instructions provided by your healthcare team.
- Stay near a bathroom after starting the laxative, as the effects can be rapid.
- Drink plenty of clear fluids to avoid dehydration.
Proper preparation is essential. If your colon is not fully cleared, the doctor may not be able to see everything clearly, and you might need to repeat the procedure.
What happens during the procedure
On the day of your colonoscopy, you will generally be asked to arrive at the clinic or hospital with plenty of time to check in and review your medical details.
Getting ready
Before the procedure begins, you will change into a hospital gown and have your vital signs (such as blood pressure and pulse) checked. An intravenous (IV) line may be placed in your arm to administer sedation or pain relief, depending on what your doctor recommends.
The colonoscopy procedure
During the procedure:
- You will lie on your side, usually with your knees drawn up.
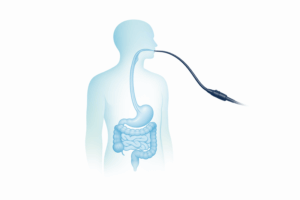
- The doctor will gently insert a thin, flexible tube called a colonoscope into your rectum. The colonoscope has a small camera and light at its tip, allowing the doctor to view the inside of your colon on a monitor.
- Air or carbon dioxide may be introduced to expand the colon and provide a better view. This can cause a feeling of fullness or mild cramping.
- If polyps or suspicious areas are found, the doctor may remove them or take small tissue samples (biopsies) using special instruments passed through the colonoscope.
- The procedure typically takes 20 to 60 minutes, depending on what is found and whether any additional procedures are required.
Throughout the colonoscopy, your comfort and safety are a top priority. Sedation helps most patients feel relaxed and often means you will have little memory of the procedure itself.
After the colonoscopy
Once the examination is complete, the colonoscope is gently withdrawn. You will be monitored for a short time as you recover from the sedation. Most people feel drowsy and may experience some bloating or mild cramping, which usually passes quickly.
Recovery and results
After your colonoscopy, you will rest in a recovery area until the sedation wears off. You should plan for someone to take you home, as you may feel sleepy or disoriented for several hours and should not drive or operate machinery.
Short-term recovery
- You may experience mild bloating, gas, or cramping for a few hours after the procedure. Walking and moving around can help relieve this discomfort.
- It is safe to resume eating and drinking once you feel ready, starting with light meals.
- Most people can return to normal activities the following day unless your doctor advises otherwise.
When to contact your doctor
While complications from colonoscopy are rare, contact your healthcare provider if you experience any of the following:
- Severe abdominal pain or persistent bloating
- Heavy rectal bleeding (a small amount of blood is normal, especially if a biopsy or polyp removal was done)
- Fever or chills
- Signs of infection or feeling generally unwell
Your doctor will advise you on what to expect and when to seek help. Most people recover quickly and without problems.
Receiving your results
In many cases, your doctor will be able to discuss the initial findings soon after the procedure. If biopsies or polyps were removed, these will be sent to a laboratory for analysis, and final results may take a few days to a week. Your healthcare team will explain what was found and what, if any, further steps are needed.
- If no abnormalities are found, you may not need another colonoscopy for several years, depending on your risk factors.
- If polyps or signs of disease are detected, your doctor will discuss follow-up care or treatment options with you.
Understanding your results and the recommended next steps is important. Do not hesitate to ask questions or request more information from your healthcare provider.
If you are concerned about symptoms like rectal bleeding or want to learn more about possible reasons for blood in the stool, our detailed guide on common causes and when to seek medical advice for blood in stool can provide further support.
Colonoscopy is a valuable tool for preventing and detecting colon problems early. While the idea of the procedure may seem daunting, most people find the process straightforward and are glad to have peace of mind about their colon health. By preparing carefully, knowing what to expect, and following your doctor’s advice, you can help ensure a smooth experience and the best possible outcome for your health.